Using Medicare
Addiction treatment is covered under state Medicare programs, though the exact terms and conditions may vary slightly based on state laws and monetary limitations.
According to MedicareInteractive.org, Medicare Part A will pay for in-patient rehabilitation services while Medicare Part B covers out-patient rehab services. MedicareInteractive.org states that the in-patient services have a lifetime limitation of 190 days if the program is not part of a general hospital; however, there is no limitation on in-patient care in a program that is part of a hospital.
Although Medicare will pay for a portion of the addiction treatment services, certain steps are required to qualify the services.
[separator top=”40″ style=”single”]
Download the Free Cost of Addiction E-Book[separator top=”40″ style=”single”]
The steps to ensure Medicare will cover the rehab program include:
- Finding a rehab program that accepts Medicare
- Getting a personal family doctor to determine that treatment is medically necessary
- Having the family doctor set up the treatment plan
A family doctor will need to refer individuals to the program before it is possible to get the treatment. Once the doctor establishes that treatment is medically necessary, Medicare will pay the same percentage that is covered under a hospital stay for other medical treatments.
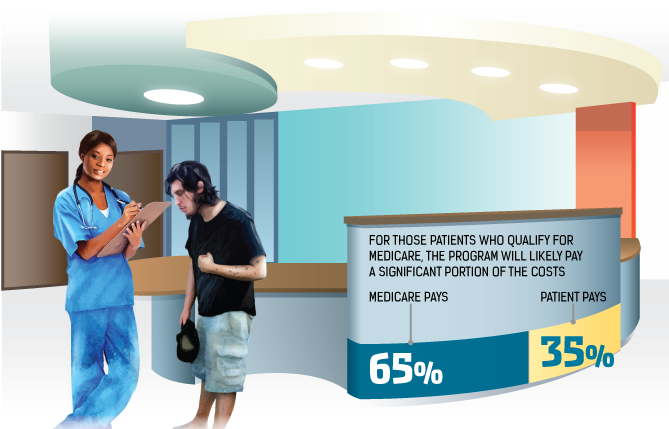
Medicare will pay for out-patient services that are approved by the program; however, the program does limit the total payment to 65 percent of the cost. Individuals are required to pay for the other 35 percent of out-patient addiction treatment.
The cost of addiction treatment may seem impossible to overcome, but options are available to help pay for the treatment. Even if a personal insurance plan does not cover addiction treatment, alternative payment solutions can make treatment affordable for any budget.
